Quick Start
Refer to the Eligibility API Best Practices and Workflow guide. The API Workflow section in the left pane in the developer portal provides information about the required API workflows.
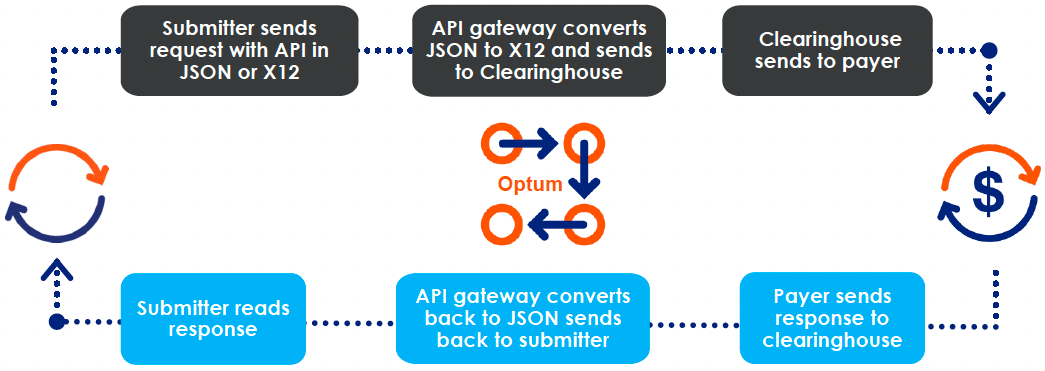
Data Flow Process
First-time users
In addition to API Reference and Guides, our developer portal provides the following resources:
- Required fields
- Format of the returned response
- Error formats
- Examples
- Downloadable OpenAPI specification in the API Reference >> API product >> Overview section
Things to do
- Visit our Marketplace to explore our products.
- Based on your business type, subscribe to the product of your choice to familiarize yourself with our APIs before contracting to integrate our APIs for real-time API testing in your production environment.
- Create a sandbox account without any financial obligations.
- Generate a Bearer token.
- Try our APIs in Try It interface or in your development platform using the predefined fields and values.
IMPORTANT
The sandbox returns a canned response based on the received data. There is no validation check or confirmation of specifically required information. These checks would only occur in the production environment. You would need to manually review the companion guides offered by the specific payers to confirm what is required for each.
Explore how the JSON-to-EDI API Mapping works.
After you have tested and selected the product for your business type, you are ready for transiting to production environment.
Contract for production environment
Contract with us and procure your production credentials from your Optum representative.
TIPS
- Use the quick reference list (highlighted in a green arrow below) link in the developer portal to search for specific information that you are looking for.
- Use the API examples in every API collection in the developer portal (highlighted in pink arrow below) to search for an API example.
- Use the Glossary (highlighted in orange arrow below) to look up the terms and their definitions.
- Use the left navigation (indicated by the red arrow below) for topic-wise help covered in this developer portal. Scroll down to view all of the product documentation.
Or
Click one of the product blocks (indicated by blue arrow below).
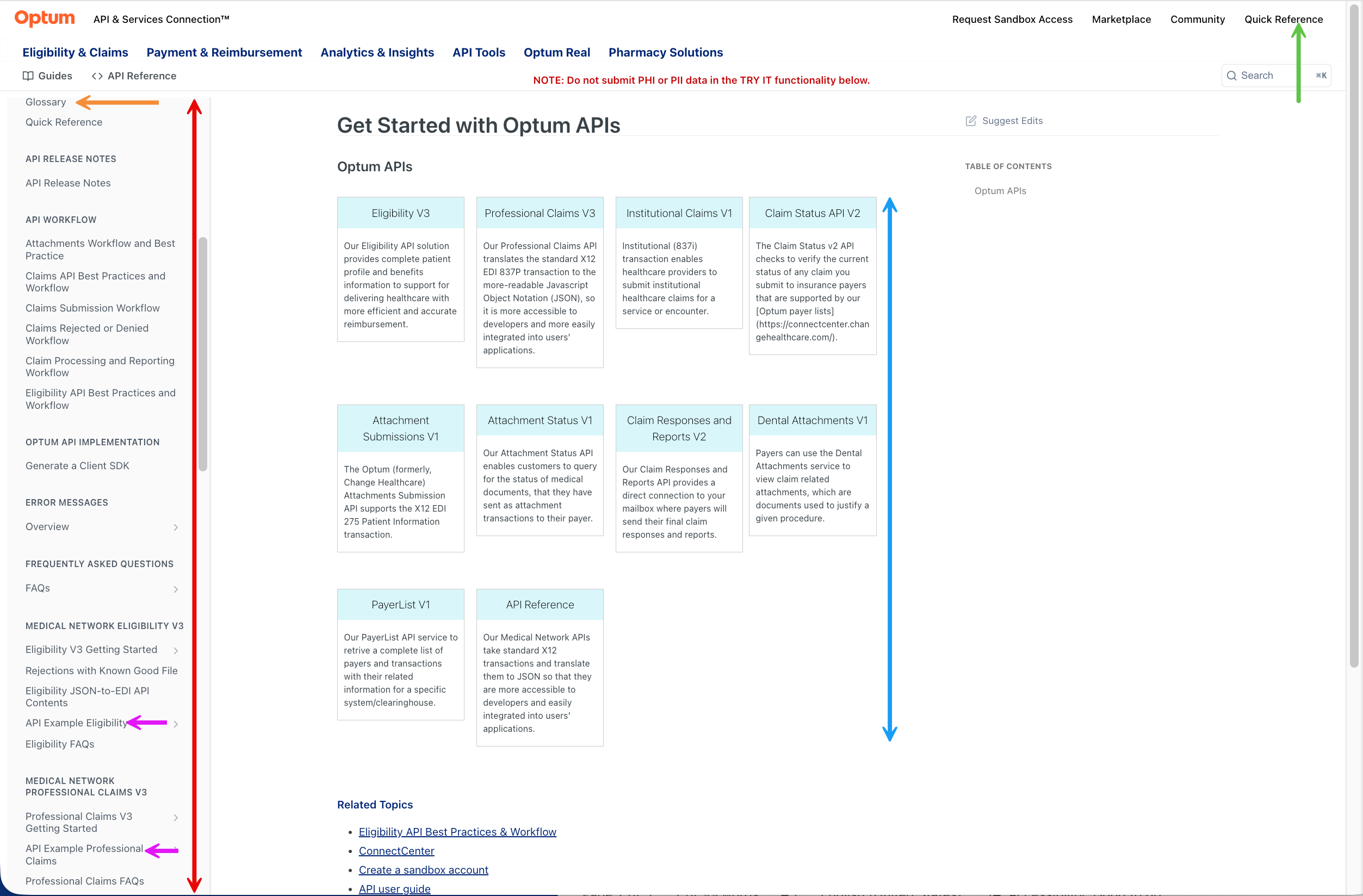
Dev Portal Getting Started
Browse by product
| 🔴 Attachments Submissions |
|---|
| The Attachments Submissions v1 API allows clients to submit claim attachments and query their status. Attachments submissions take two forms: Solicited and Unsolicited. Solicited claims usually are sent by payers to providers requesting documentation for a claim. The API supports the X12 EDI 275 Patient Information transaction. It translates this standard to JSON, so it is more accessible to developers for integration into users’ applications. 📖 API Guide ✍️ API Reference |
| 🔶 Attachments Status |
|---|
| The Attachments Status v1 API enables customers to query for the status of claim attachment transactions (typically sending of medical information attachments) submitted to their payer. The API takes the transaction details and returns status information in a format that is understandable to the customer. 📖 API Guide ✍️ API Reference |
| 🔴 Attachments Retrieval The Attachments Retrieval v1 API lets you search and download claim attachments documents for payers. It has search options based on date range, claim number, memberId, patient first name, and last name. This API supports legacy (formerly Emdeon) network connections. For a full list of Legacy RelayHealth network connections, please visit ConnectCenter.📖 API Guide ✍️ API Reference |
| 🔵 Claims Status |
|---|
| The claim submitter uses a Claim Status v2 API request to inquire about the status of a previously submitted claim. If the claim is finalized, the response provides the disposition of the claim (for example, Paid, or Denied). For Denied or Rejected outcomes, the response includes the reasons for the denial or rejection. The payer returns the response, as an X12 EDI 277 transaction, which is translated back to JSON by the API gateway. It translates this standard to JSON for developer accessibility and integration into users’ applications. 📖 API Guide ✍️ API Reference |
| 🔵 Claim Responses & Reports |
|---|
| The Claim Responses and Reports API provides a direct connection to your mailbox where payers will send their responses and reports to your claims. Retrieve valuable claim responses and reports from payers. 📖 API Guide ✍️ API References |
| 🔶 Eligibility |
|---|
| The Eligibility v3 API provides complete patient profile and benefits information to support healthcare delivery and more-efficient and accurate reimbursement. Providers get better front-end information to improve claiming processes and reimbursement rates. For payers, claims spend less time in pending status and a fewer rejected and reworked claims. It makes this popular EDI transaction set more accessible to developers and users’ applications. The API uses the standard X12 EDI 270 eligibility transaction, and formats it in JSON for an HTTP request. We manage the X12 standards in the background, and give you efficient access to medical subscriber or dependent plan membership, copays, coinsurances, deductibles, and more in an easy-to-use, human-readable format. 📖 API Guide ✍️ API Reference |
| ⚫ Institutional Claims |
|---|
| The Institutional Claims v1 API enables healthcare providers to submit institutional healthcare claims for a service or an encounter. A healthcare claim includes patient information, related diagnoses, procedures performed or services provided, and any related charges. This product allows for significant savings in time and a higher propensity for acceptance on the first submission. 📖 API Guide ✍️ API Reference |
| ⚫ PayerList |
|---|
| Use the PayerList service to complete list of payers and transactions with their related information for a specific system/clearinghouse. 📖 PayerList Guide ✍️ API Guide |
| 🅾️ Professional Claims |
|---|
| Professional (837P) transaction allows physicians and other medical service providers to submit healthcare claims for a medical service or encounter. The Professional Claims API takes the standard established in the X12 EDI 837P transaction and translates this standard to JSON so it is more accessible to developers and easily integrated into users’ applications. 📖 API Guide ✍️ API Reference |
| 🟢 Dental Attachments |
|---|
| The Dental Attachments API provides the capability to send attachments data (including but not limited to X-Rays, EOBs, Charts, and so on), to Optum Dental electronically. This data will include claim demographic (payer, provider, patient, and service) details, and attachments related information. 📖 API Guide ✍️ API Reference |
Support
NEED HELP?
If you have a specific question and need a separate call:
- send us a message Here
or- for other modes of communication, review our support and escalation guide
or- visit our interactive developer community and sign up to access several learning resources
Resources
📹 Developer tutorials
🏢 Office hours support sessions
Related Topics
Updated about 1 month ago