Professional Claims FAQs
NOTE
Medicare payers accept claims only for subscribers. If you want to submit a dependent claim with a Medicare payer, submit the dependent as a subscriber in the claim request.
How do I access the Professional Claims APIs?
Providers use the Professional Claims APIs to submit their medical procedure claims to their payers.
- API environments
- Try our APIs
- API URLs
- Use the
/professionalclaims/v3/validationendpoint to check your request:
The /validation endpoint does not send your transaction to the payer. It checks for the correct well-formed syntax of your submission. It does not check the accuracy of the information included in your submission, so you must separately ensure that the claim is complete and accurate before submission.
NOTE
The
/validationand/submissionendpoints use the same request model. Avoid sending any claims until you have tested your submission process and validated your claim!
What information goes in the API Request header?
Please see example in API Request Header.
How do I check the Operating Status of the API?
Our /professionalclaims/v3/healthcheck endpoint checks the operating status of the Professional Claims API engine. Please see API example
Do you have a sandbox that I can test with before signing a contract?
Yes, we do. See Sandbox FAQs and API environments.
What does a typical Professional Claims API request look like?
The Professional Claims API uses a POST request. Responses to our Medical Network APIs can be lengthy due to the many data points that a payer or trading partner provides in the query response. Professional claims can have up to fifty line items (Loop 2400) in the claimInformation object (Loop 2300 in the EDI spec), each of which, reflects payer decisions on payment.
Our APIs translate back-and-forth between JSON and X12 EDI when the information departs into and returns from the medical network. All fields and JSON objects conform to the EDI 837p transaction standard.
Professional Claims API request example
Please see API example.
✍️ In the sandbox request, using value: test00005 (lower case and not uppercase), for
fieldName: patientControlNumber returns EDITS canned response.
Example Claim JSON objects
Please see API example.
What do Professional Claims Validation API responses look like?
Please see API example.
What is the claimReference field in the Submission response?
The claimReference field is an object containing the list of identifiers that you can use to track a claim. If questions arise about a claim, you can provide the information listed in the claimReference object to Optum support for troubleshooting purposes. It appears in all submission responses for claims. The list of identifiers may differ depending on the context for the response. Please see API example.
claimReference object fields
claimReference object fieldsPlease see Response Contents - Professional Claims.
If the Primary claims are sent electronically, will the Secondary/Tertiary claims be sent electronically as well all the time?
For the secondary claim to be paid electronically, the primary payer must accept secondary claim.
Do you bill for a failed claim due to technical error?
Every transaction that makes it to the clearinghouse is billable. All errors at the API level, and some errors at the ingress of the clearinghouse, are considered non-billable.
What's the difference between a Professional claim and an Institutional claim?
- Professional billing typically uses the 837p transaction (or the CMS-1500 form in hard copy)
- Institutional billings use the 837i transaction
We support both types of electronic claims and transactions. Institutional billing also sometimes encompasses collections while Professional Claims and billing typically do not.
Professional billing controls the billing of claims generated for work performed by physicians, suppliers, and other non-institutional providers for both outpatient and inpatient services. One commonality: our APIs help support and automate insurance coding for both Institutional and Professional Claims.
A provider has two different teams; one enters the claim and the other verifies and submits it. Before submitting, can they enter the claim, save it and have it released when ready?
Our APIs do not have a caching/drafting feature. Customers can develop and automate this feature. Customers should hold the claims at their end, and programmatically set up a console to separate working on claims from submitting them.
How many line items can be on a single claim?
A single professional claim supports up to 50 service line items (serviceLine).
Are there guidelines for predicting the rate of unique claims submitted for a practice?
Rates of unique claims are isolated to each individual provider. Every provider is different. Whenever you render a medical service, file a claim.
Where can we include the information about the primary claim on the API request for the secondary claim?
Send any payer-specific information in the otherPayerName object. Use otherSubscriberInformation to convey details for the member specifically. For more information Professional Claims JSON-to-EDI Contents.
Are there any other fields in the request body of the Professional Claims to be aware of?
Yes, we have included examples of Prof. Claims request contents and Response Contents - Professional Claims.
How to send an EOB from the primary payer with the claim?
Secondary claim information goes in to loop 2320. We do not have any documentation on what is required for secondary claims since that is a billing-specific question. Also, if you want to send the EOB to the payer, you should work with them directly to determine how you want those submitted. To learn more about Billing or Invoice Assistance, check out the last page of the Support & Escalation Guide.
What would be the correct co-insurance amount for Professional (Physician) Visit — Office, for example, for Professional (Physician) Visit — Office but one says 0% and the other says 10%?
Service Types: Professional (Physician) Visit — Office is the correct amount. The other serviceType codes are not Professional Visit and would have a higher percentage based on that payer's response.
Why is the Claim Submission API giving 400 error for the test values?
Error 400 means, there is a missing or invalid data or parameters in the request. Here is a listing of HTTP error response codes.
Do you support appeals for denials? Are there any APIs through which these appeals can be submitted?
If a claim is denied or partially paid by a payer, a corrected claim should be sent for additional review. Submitting a corrected claim would require the claim frequency code '7', and the payer claim controlNumber must be included on the claim in the claimControlNumber field in the claimSupplementalInformation.
The claimControlNumber is the number assigned by the payer to identify a claim. Once submitted, the payer will review the claim and make any changes based on their internal review. The claimControlNumber is found on the payer 277 report. The same process would need to be followed for voided claims, but using a frequency code '8'. Please see a sample corrected claim in API example.
How do you re-submit a claim that was denied – Appeal & Denial
Please see API example.
Is it possible to submit multiple claims at once, in batches?
We do offer batch submissions through SFTP only, our current API does not allow for batch submissions. These would have to be 5010-compliant EDI files. Please reach out to your sales representative to discuss pricing options for SFTP submissions.
When a claim is submitted via the API, the API returns a claim ID. What API can I use to fetch the payer's claim number before we receive the ERA, ideally the next day after the claim is submitted successfully?
The payer-assigned claim ID would be returned through the SD and SF reports mapping we provide through the Responses and Reports v2 API. Additionally, you may be able to check the provider portal for the payer for this information.
Can we make multiple claims in one API call? If so, which endpoint should we use?
This is not possible through the current APIs. Only single submission is allowed. You can submit batch through SFTP but the batch file would need to be in X12 formats. Here is the available Claim Responses and Reports documentation that describes the available reports.
I am developing an application that will replace the old paper forms and start using the Professional Claim API. I cannot find the Prior Authorization Number.
- Open the Professional Claims OpenAPI spec.
- Do a Ctrl + F and search for priorAuthoriationNumber (under ClaimSupplementalInformation) in the spec shown as below.
"priorAuthorizationNumber":{"type":"string","description":"Loop: 2300, Segment: REF, Element: REF02 and REF01=G1"}
How to handle multiple authorization numbers per claim?
If the Institutional Claims required multiple authorization numbers, multiple claims need to be submitted. Submission through the Professional API allows for prior authorization information to be submitted at both the claim and line level Institutional Claims APIs allows for prior authorization information to be submitted at the claim level only. Please see example below.
Here is a sample from our Open API Specs.
ServiceLineReferenceInformation:
type: object
properties:
repricedLineItemReferenceNumber:
type: string
description: 'Loop: 2400, Segment: REF, Element: REF02 Notes: When REF01=9B'
adjustedRepricedLineItemReferenceNumber:
type: string
description: 'Loop: 2400, Segment: REF, Element: REF02 Note: When REF01=9D'
priorAuthorization:
maxItems: 5
minItems: 0
type: array
description: Loop 2400 REF
items:
ClaimSupplementalInformation:
type: object
properties:
reportInformation:
$ref: '#/components/schemas/ReportInformation'
priorAuthorizationNumber:
type: string
description: 'Loop 2300; Segment: REF; Element: REF02 when REF01 = G1'
I sometimes get back errors from the payer like: "Loop 2310B (rendering provider name) is missing, it is expected to be used when loop 2420A is used with the same value in every loop 2400". How can I send the rendering provider in loop 2310B?
See Provider object in Request body parameters.
For EDI claims, where can I put the session times in Loop 2400 for each individual line in the claim request when using the claims API?
Look up Loop 2400 in Professional Claims JSON-to-EDI Contents to view different SV segments.
How to avoid the error "Other Payer Primary ID# is Missing or Invalid" when the other payer doesn't have a payer ID and for which the claims are set up to be sent by paper?
The CPID for paper claims are listed here:
Professional 1500 form (Medical Claims):
- Commercial CPID 4320
- Medicaid CPID 4322
- BCBS CPID 4323
Institutional UB-04 form (Hospital Claims):
- Commercial CPID 4350
- Medicaid CPID 4352
- BCBS CPID 4353
What is Professional Claims API and what is it used for?
Please see Professional Claims V3 Getting Started.
I am trying to test out a scenario where the clinic would enter a specific service type code and want to get patient benefits for that specific service code?
All of our sandbox API values and test responses are real payer responses that have been de-identified and emulated. The only value that affects the response in sandbox is the tradingPartnerServiceId. You can receive different responses by switching that out, but the responses will not vary if you change other values, such as the serviceTypeCode.
Is a list of Eligibility AAA errors with a description available?
Yes, here is a list of AAA error codes requests and possible resolutions .
Does the Revenue Performance Advisor work with claims submitted with the API as well as claims submitted through the revenue advisor interface?
Only the Eligibility API works with Revenue Performance Advisor. Our claims APIs currently route to another one of our switches, this will be considered for a future enhancement.
My client would be billing her clients for the visit which is not a professional/specialist visit but more like evaluation and management services that come under CPT 99214. Other than 98 (Professional physician visit-office), any other code I can use?
Include serviceTypeCode 30 to pull back all benefit information.
What is the Claim submission flow?
Please see example in Claim Submission workflow.
Do we need to use same control ID for a claim in submission and checking its claim status?
The controlNumber should be unique for each individual submission.
How can I add modifiers to the services/procedures/other codes of a claim? How can you express that a CPT code had to be added to a claim so that the payer have sufficient support or their adjudication?
Please see the following example for mapping for submitting modifiers. In an instance where a code needs to be added to a claim, a corrected claim should be submitted. This would require the claim frequency code '7' to be submitted, and the payer claim control number must be included on the claim in the claimControlNumber field in the claimSupplementalInformation. The claimControlNumber is the number assigned by the payer to identify a claim. Once submitted, payers will review the claim and make any changes based on their internal review.
ProfessionalService:
required:
- compositeDiagnosisCodePointers
- lineItemChargeAmount
- measurementUnit
- procedureCode
- procedureIdentifier
- serviceUnitCount
type: object
properties:
procedureIdentifier:
type: string
description: >-
Loop: 2400, Segment: SV1, Element: SV101-01, Notes: Allowed Values are:
- 'ER' Jurisdiction Specific Procedure and Supply Codes,
- 'HC' Health Care Financing Administration Common Procedural Coding System
(HCPCS) Codes, 'IV' Home Infusion EDI Coalition (HIEC) Product/Service Code,'WK' Advanced Billing Concepts (ABC) Codes
example: HC
enum:
- ER
- HC
- IV
- WK
procedureCode:
- type: string
- description: 'Loop 2400, Segment: SV1, Element: SV101-02'
- example: E0570
procedureModifiers:
- maxItems: 4
- minItems: 0
- type: array
- description: >-
Loop 2400, Segment: SV1, Elements: SV101-03 to SV101-06, Notes:
Required when modifier clarifies or improves the reporting accuracy
of the associated procedure code. If not required then do not send
items:
- type: string
description:
- type: string
- description: >-
Loop 2400, Segment: SV1, Element: SV101-07, Notes: A free form
description to clarify teh related data elements and their content
Can the modifier code be added to the first submission or I need to submit another claim with frequency code 7, just to add the modifier?
We are not able to say if a code would be 'required'; it will vary from payer-to-payer. However, you can add a modifier to the initial claim in the professionalService object from the Professional Claims JSON-to-EDI Mapping Guide's procedureModifier.
Provide the source to obtain the master list related to CMS1500/UB04 Claims forms.
- 1500 is a medical claim (Professional)
- UB04 is hospital claim (Institutional)
- 837P is a 1500 Medical Claims
- 837I is a UB04 Hospital claims
When paper is sent, a 1500 form is used for Medical claims and UB04 for Hospital. We do not have a master list of information. The information is common across the medical industry and there are many crosswalks or sites you can find, which map the paper claim locations to a 837.
Is there any field other than the patient_control_number field in claims payload that can associate the Claims to the ERA? I need the field to come back in the ERA.
The patientControlNumber is typically the main identifier, which is used in tracking claims through to payment. The Patient Control number can be up to 38 alphanumeric characters, and should be unique per submission. Additionally, you can submit a providerControlNumber (API KEY)/LINE ITEM CONTROL NUMBER (5010 X12). The providerControlNumber must be unique within a patient control number. Payers are required to return this number in the remittance advice transaction (835) if the provider sends it to them in the 837. However, please note this is dependent on the claim adjudication being done on a service line level basis.
Are the address1 and City fields, which are part of the payerAddress object necessary when submitting the claim? Where can the address information be obtained for the payers listed in the ConnectCenter Payer list?
The payer address is not required when submitting claims electronically. The payer address information is required only if a claim was intended to be submitted through paper. We route transactions based on the CPID, which is the tradingPartnerServiceId submitted in the request.
Do we need to be enrolled at Remitter to receive 277 Claim Status? We have enrolled through ConnectCenter as a Submitter, is 277 claim status response dependent on us being enrolled as the Remitter for a payer?
See Claim Status FAQs.
Claim Status responses are not dependent on being enrolled for Remittance.
There are two types of 277 Claim Status responses, solicited and unsolicited:
A solicited 277 would be a response from the payer to a submitted claim status request through the API. Depending on the payer, this can either be returned in a real-time response or it would be received in a batch file. If the 277 is received through batch, the response would be returned through the Responses and Reports API as an X3 file-277 Claim Status Response Data File (X12 format, JSON conversion available) – this report returns the solicited claim status X12 raw data that matches exactly what is returned by the payer and can be translated into JSON. This file is received from payers when claim status is requested and not returned in real-time. Please see example in Solicited Attachments transaction and Solicited Attachment Response to a 277R transaction.
An unsolicited 277 response would be returned through the Responses and Reports API in a SF file-Payer Report Data File (Pipe Delimited) – this report is a proprietary pipe delimited file that returns claim level payer acceptance and rejections. Please see example in Unsolicited Attachments transaction and Unsolicited Attachments for a 275 Claim transaction.
The SR you received is the human-readable version of the SF report mentioned above.
Please keep in mind that 277s will only provide information up to the point when the claim has been processed. Most payers will not provide payment details through Claim Status. For more information, see difference between solicited and unsolicited attachment.
Is the usageIndicator field validated by the clearinghouse and/or payers? Is submitting real data with a "T" usageIndicator value a valid way to test production data without actually submitting it for processing? How is this field interpreted?
Yes, sending a claim with the "T" usageIndicator is a valid way to test production data without submitting for processing. For more information, see Test Production Data without Submitting for Processing.
Invoking the submission API shows "invalid_request" as response.
Please make sure that the API you are trying to test is added to your sandbox entitlement/credentials. And please remember that within the sandbox environment, you can only test with our sandbox API values and test responses. With claims, you can do more thorough testing with live data being sent to the production endpoint, but be sure to specify the usage indicator to 'T' (test). The JSON would be: usageIndicator: "T". This way, it will not go to the payers.
Either organizationName is null or lastName and firstName is null. If lastName and firstName is not null, middleName may or may not be null?
This issue might be due to either the organization or individual provider information being sent on a transaction. Only one of these sets is allowed per provider object, you would need to send either the organization or individual provider (first name, last name) not both for the same provider object.
Is there a page that shows how to generate different error responses while using professional claim validation API and professional claim submission API?
The /validation endpoint does not send your transaction to the payer. It checks for the correct well-formed syntax of your submission. It does not check the accuracy of the information included in your submission, so you must separately ensure that the claim is complete and accurate before submission. The /submission endpoint would be the primary method of test claim data. If you submit usageIndicator: "T", the production transition will be flagged as a test claim and will not be sent to the payer.
What is diagnosisCodePointers in compositeDiagnosisCodePointers object in professional claim validation API?
The Diagnosis Pointer relates to the reason for which the service was performed. This first pointer designates the primary diagnosis for this EQ segment. Remaining diagnosis pointers indicate declining level of importance to the EQ segment. Acceptable values are 1 through 8, and correspond to Composite Data Elements 01 through 08 in the Health Care Diagnosis Code HI segment in loop 2100C. A maximum of four diagnosis pointers may be entered per line. For example, in the following snippet: "compositeDiagnosisCodePointers": {"diagnosisCodePointers": ["1", "2"], the first pointer designates the primary diagnosis for this service line and the remaining diagnosis pointers indicate declining level of importance to service line. Up to 8 CPT codes can be sent.
You can find more information here.
Is it necessary to integrate the payer enrollment API also to launch an end-to-end claims and billing feature?
Enrollments for customers using the Medical Network APIs are submitted via our ConnectCenter under Payer Tools >> Enrollment Central. If you are unable to login to the application, please reach out to ConnectCenter MFA Support: 800-527-8133 opt., 7 or [email protected].
When trying to determine if a specific payer requires enrollment, this can be found on our payer list . The Exchange Claims & Remittance Payer List contains a list of all of the active payers for those transaction types. Once downloaded, please locate the Enrollment (if enrolling after 2/21/2024) column. A "Y" would indicate that an enrollment is required for the associated payer ID/CPIDs.
While using the Professional Claims submission API, the claim submitted as against the one in ConnectCenter, some information is missing: Patient information and the payer name is listed as "unknown". Do I have the patient be referred to the "self" code in the " relationshipToSubscriberCode field?
relationshipToSubscriberCode field?The payer name will populate as unknown unless the tradingPartnerName is sent along with the specific trandingPartnerServiceId. Please add this to future submissions and the payer name will populate in ConnectCenter.
Regarding the missing patient information, if the patient is the subscriber, only the subscriber details would be present in the transactions. The patient information is used if the patient is a dependent of the subscriber.
- Subscriber (can be the patient when the patient is the subscriber or is considered to be the subscriber)
- Dependent (patient, when the patient is not considered to be the subscriber)
What are the possible values for status and customerClaimNumber fields in the Professional Claims Submission response body?
The possible response values will be the claim status category codes and the claim status codes (both published by the X12 Organization).
The codes are the same whether the claim is Professional or Institutional.
As for the customerClaimNumber, we would to see that being returned in an actual response for us to look at it further. We've been unable to locate that field being populated on any SF report we've looked at.
The status field encodes both claimStatusCategoryCode and claimStatusCode. They are separated by a colon as shown in this example SF report.
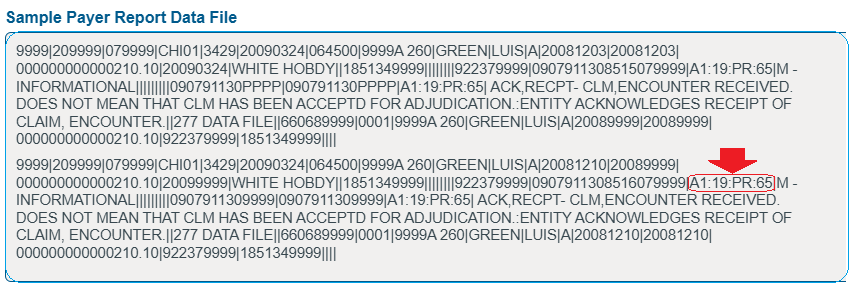
Set 1: claimStatusCategoryCode = A1, claimStatusCode = 19
Set 2: claimStatusCategoryCode = PR, claimStatusCode = 65
Related Topics
Updated about 2 months ago