This page contains information about new features, enhancements, regulatory updates, and any issues or defects that have been addressed from the previous version of the product.
Release Notes V5.1.3
- As part of this release, we are now supporting Real Document Search APIproviders can securely retrieve claim- and payment-related documents, offering quick access to key information for reconciliation, review and recordkeeping. This centralized API provides access to documents such as EDI 835, provider remittance advice (PRA) notices, explanations of benefit (EOB), provider letters and virtual card payment (VCP) documents. This helps enable providers to efficiently locate and retrieve files, helping reduce time spent on administrative tasks and enhance the provider experience.
Through a single, centralized API, providers can access claim information in real time, including:
Document Metadata
Secure document download
- Payer ID updates have been made to the Claim Actions documentation and db to align with the latest schema guidance provided by UHC, ensuring consistency and clarity across systems.
- The Subscribed API view in the Optum Real UI has been enhanced to clearly differentiate APIs based on their enrollment and processing status, improving clarity and usability for users managing multiple APIs.
APIs are now categorized into three distinct sections:- Selected APIs: Displays only APIs included in the current order.
- Subscribed APIs: Displays APIs for which enrollment has been successfully completed.
- Processing APIs (APIs In Progress): Displays APIs that are currently in an enrollment or processing state.
Release Notes V5.1.2
- As part of this release, we are now supporting Real Prior Auth/Referral Actions API where providers can submit, track and manage prior authorization and referral requests. By streamlining prior authorization and referral requests before care is delivered, this centralized API helps providers reduce denials and decrease surprise bills for patients.
Through a single, centralized API, providers can access claim information in real time, including:- Prior authorization submission and status
- Referral submission and status
- Supporting documentation submission
Release Notes V5.1.1
Enhancements
-
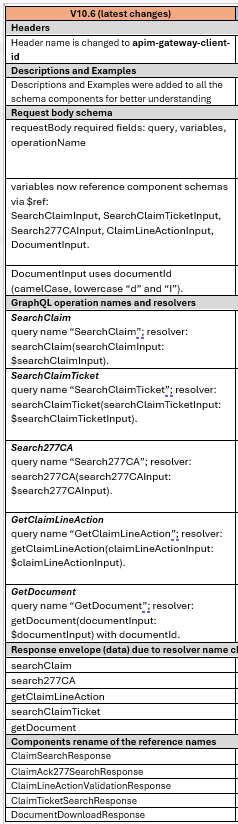
As part of this release, Real Claim Inquiry API has been updated with V10.6 schema changes.
Release Notes V5.1
Enhancements
- As part of this release, Real Patient Benefit Check API has been updated to support benefit category and benefit language operation.
Release Notes V4.1.2.1
Enhancements
- As part of this release, Real Patient Benefit Check API schema changes have been implemented. The data dictionary is updated with all the changes in Technical reference guide.
Release Notes V4.1
Enhancements
- Updated tool tip in Optum Real Hub UI for 'Claim Number' to indicate "Please use the Patient Control Number from the 835 remittance".
- Payer registration step 1 screen been updated to remove payer selection and update text to reflect prefilled TIN from Optum AI Marketplace.
The new design introduces revised verbiage for multiple states in the workflow, including:
Success State: “You’re All Set” → Updated with clear instructions to return to Optum AI Marketplace.
Already Enrolled State: “TIN Already Enrolled for Selected API(s)” → Updated with step-by-step guidance for next actions.
Enrollment Failure State: “Enrollment Couldn’t Be Completed” → Updated with instructions for creating a new purchase excluding already enrolled APIs.
Information Collected State: Updated to remove payer-specific references and clarify next steps.
Resolved Issues
- Resolved a design issue where Sign out button was going out of frame in certain scenarios.
- Resolved a issue where The Pre Service Eligibility request schema was not updated for PCPhistorylist from object type to array list.
Release Notes V4
Enhancements
- As part of this release, Referral Inquiry capability is available as part of the Real Patient Benefit Check API.
- As part of this release, we are now supporting the Real Claim Actions API providers can now submit more accurate claims, reconciliation requests, appeals, and supporting documentation at the point of billing.
Through a single, centralized API, providers can access claim information in real time, including:X12 claim validation (HIPAA) Membership coverage eligibility for the date of service Coordination of benefits including primacy and coverage details Prior authorization requirements and status Claim submission Reconciliation request and appeal submission Supporting documentation submission - As part of this effort Order status now gets updated based on Order ID and status inlcuded as part of a call.
- As part of this effort we are now providing the ability to update TIN details.
- As part of this release Pre Service Eligibility API has been updated to reflect below changes:
- Update to full eligibility query.
- New Objects and fields added as part of response:
a. paidThroughDate (New Field), consumerName (New Field) under insurance info object
b. primaryCarePhysician.pcpHistoryList: (New Object)
c. serviceLevels.vendorServices: (New Array )
d. fundingArrangementDescription (New Field)
e. medicaidVariables: (New Array)
f. messages: (New Array)
Resolved Issues
- Resolved an issue where payer name and provider name could be passed in the request header.
- Resolved an issue where the Claim-Inquiry service was experiencing issues with schema mapping for getClaimLineAction and getDocumentSchema.
- Resolved an issue where Claim enrichment flow incorrectly proceeds to ACE instead of failing and returning error response on enrichment errors.
Release Notes V3.2
- An error message will now be returned when the Payer ID passed as part of the request does not match the Payer ID included in the X12 request. This change was made to the Real Claim Pre-Check API and the unreleased Real Claim Actions API.
- Clear validation error messages will now be returned when requests are submitted with missing or invalid required parameter.
- United Healthcare TIN consumption logic has been enhanced to accept Excel files with any number of columns and process the required columns into the database without error.
- The Optum Real hub UI screen has been enhanced to display previously subscribed APIs by the provider.
Release Notes V3.1
- Resolved an issue where clients subscribed Real Preservice Eligibility API were unable to use sandbox for live data testing.
Release Notes V3
- As part of this release, we are now supporting the Real Patient Benefit Check API, which helps providers validate patient benefits as well as prior authorization and referral requirements before care is delivered. This API allows you to reduce denials and give patients clear answers about what’s covered and what they’ll owe before they receive care, helping reduce surprise bills and improve patient satisfaction. Through a single, centralized API, providers can check patient's:
- Prior authorization inquiry
-Prior authorization in file
-(Coming soon) Benefits by CPT code
-(Coming soon) Referral inquiry
-(Coming soon) Benefit languag
Release Notes V2
- As part of this release, we are now supporting “Real Claim Inquiry API” where providers can receive real-time updates on submitted claims to make informed decisions regarding reconciliation requests and appeals to help reduce administrative burden. Through a single, centralized API, providers can access claim information in real time, including:
- Claim summaries and details - Status at the claim and service level - Available actions for reconciliations and appeals at the service level - Download of associated documents - Addition of post-purchase test environment
- Once the API purchase status shows “subscribed” in the AI Marketplace account, customers can use their existing sandbox credentials to send live data to a sandbox environment for the API they have purchased.
- At that point, responses will be based on the live data submitted to the sandbox environment as opposed to mock data preloaded to the sandbox environment.
-The customer will retain the ability to query mock responses from sandbox environment by using an optional request header called “environment” by placing the value “sandbox’ in the optional header.
NOTE: Do not submit PHI or PII data in the TRY IT functionality below.
Release Notes V1
- As part of this release, we are now supporting “Real Pre-Service Eligibility API” where providers can access eligibility data across multiple payers directly within their existing workflow, including:
-Eligibility information including patient demographic information, plan-level cost shares, plan coverage details and insurance details -Coordination of benefits including primacy and coverage details for each payer plan -Image of a patient’s insurance ID card -Provider In and Out of Network status - As part of this release, we are now supporting “Real Claim Pre-Check API” where providers can validate claim data directly within existing workflow, including:
-X12 claim validation (HIPAA)
-Membership and coverage eligibility for the date of service
-Coordination of Benefits (COB) including primacy and coverage details for patient
-Prior Authorization (PA) requirements and status
-Adherence to payment and medical policies